What Are the Types of Depression?
Depression is characterized by persistently low mood and lack of interest in activities. Learn about the different types of depression in this article.
What Is Depression?
Depression is a mental health illness that impacts how a person thinks and feels. Depression causes feelings of sadness and a lack of interest in previously enjoyable activities. It can lead to various mental and physical issues and negatively impact the ability to function at work, school, or home.
Depression is one of the leading causes of disability worldwide. An estimated 280 million people are affected, including approximately 5% of the adult population and 5.7% of older adults sixty or over. At least 10% of people in the U.S. will experience depressive disorders at some point in their lives.1

Contact Profound Treatment to Learn More
Our team is standing by to discuss treatment options with you. Your call is completely confidential and no obligation is required.
Is Depression Genetic?
Depressive disorders can be determined by a combination of genetic and environmental factors. A team of researchers isolated a genome-wide connection to chromosome 3p25-26 that appears to be prevalent in multiple family members with recurrent, severe depressive disorders. Scientists believe that as many as 40% of individuals with depression have some genetic link.2
In addition, women are more likely to develop depressive disorders than men. It was reported that women had a 42% chance of having a hereditary depression-related disorder versus 29% of men.3
Clinical Depression: an Overview
Depression Symptoms
Symptoms of depression can be mental, physical, and social. Common signs and symptoms of depression may include:
- Persistent depressed mood or feelings of sadness for most of the day, nearly every day
- Feelings of anxiety and/or restlessness
- Feeling hopeless, worthless, and pessimistic
- Excessive crying
- Feeling bothered, annoyed, irritated, or angry, even over minor concerns
- Loss of interest in hobbies and interests once enjoyed
- Decreased energy or fatigue
- Isolation
- Avoiding contact with others
- Sleep disturbances, including insomnia or sleeping too much
- Trouble thinking, concentrating, or remembering
- Unexplained physical problems, such as headaches, stomach pain, or back pain
- Frequent or recurrent thoughts of death, suicide, or suicide attempts
Depression vs. Sadness/Grief
Depression differs from sadness or grief in that normal feelings of sadness resolve after a period of time, whereas depressive symptoms are persistent and negatively impact self-esteem, creating feelings of worthlessness and hopelessness. Similarly to depression, grief can be ongoing but is a normal response to a life event.
Depression and grief can be experienced concurrently; however, their strength, intensity, and duration are what set them apart. In depressive disorder, symptoms are persistent for two weeks or more. With grief, the painful feelings may come in waves that include feelings of happiness over positive memories.
What Does Life With Depression Look Like?
Common Types of Depression
There are several types of depression. The symptoms of each depressive disorder may show up in different ways and exhibit a variety of distinct symptoms.
Major Depressive Disorder (MDD)
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), in order to receive a diagnosis of major depressive disorder, an individual must experience five or more of the symptoms during the same two-week period, and at least one symptom should be either depressed mood or loss of interest or pleasure.
The average lifetime prevalence of MDD is about 12%, and the prevalence rate is almost doubled in women as opposed to men. Further, major depressive disorder occurs more often in individuals with no close interpersonal relationships and who are divorced, separated, or widowed. While statistics reveal no difference in prevalence among races and socioeconomic status, MDD is reported more frequently in rural areas than urban areas.5
Persistent Depressive Disorder (PDD)
Persistent depressive disorder, previously known as dysthymic disorder, is a continuous, chronic type of depression. PDD is a complex depressive disorder that is very similar to MDD but is often less intense and must last continuously for at least two years. At one time, PDD was classified as a depressed personality disorder.
To be diagnosed with PDD, one must experience a depressed mood throughout most of the day, more often than not, for at least two years, and does not meet the criteria for major depressive disorder. The depressed mood must also be followed by two or more other symptoms of depression, such as low self-esteem, low energy or fatigue, noticeable changes in appetite, poor concentration, or hopelessness.
Bipolar Disorder
Bipolar disorder, previously referred to as manic-depressive disorder or manic depression, is characterized by unusual shifts, or episodes, in mood, energy level, and concentration. These episodes are defined as depression and mania, abnormally elevated feelings of excitement, euphoria, and delusions. There are three different types of bipolar disorder:
- Bipolar I disorder is often defined by episodes of mania that last at least seven days or are so severe they require hospitalization. Usually, depressive episodes also occur and last for at least two weeks.
- Bipolar II disorder is defined by a combination of depression levels with episodes of hypomania, a milder version of mania. The episodes in bipolar II are less severe than those in bipolar I; however, they still cause impairments in an individual’s life.
- Cyclothymic disorder is defined by relatively mild depression and hypomania, and the symptoms do not reach the severity of either mania or a major depressive episode.
Postpartum Depression (PPD)
Another type of depression is postpartum depression. PPD is a complex mix of emotional, physical, and behavioral changes that occur in some women after giving birth. According to the DSM-5, PDD is a type of major depressive disorder that begins four to six weeks after delivery. Postpartum depression symptoms often include:
- Trouble sleeping
- Appetite changes
- Severe fatigue
- Lower libido
- Frequent mood changes
- Being uninterested in or feeling unable to bond with their baby
- Crying all the time and often for no reason
- Severe anger
- Feelings of worthlessness, helplessness, and hopelessness
Premenstrual Dysphoric Disorder (PMDD)
Premenstrual dysphoric disorder is a health problem similar to premenstrual syndrome (PMS) but more severe. PMDD often occurs a week or two before the menstrual cycle and causes symptoms such as:
- Severe depression
- Irritability
- Anxiety
- Cramps or bloating
- Thoughts of suicide
- Lack of interest in activities
- Trouble focusing
- Low energy
- List Item
To be diagnosed with PMDD, one must exhibit at least five or more PMDD symptoms, one of which must be a mood symptom similar to a general depressive disorder.
Seasonal Affective Disorder (SAD)
Seasonal affective disorder is a common depression type that occurs during seasonal changes. In most cases, SAD symptoms often start in late autumn or early winter and persist until spring or summer. Nonetheless, some individuals experience depressive episodes during the spring and summer months, which is called summer-pattern SAD and is less common.
Individuals with SAD exhibit symptoms common in MDD, usually lasting four to five months per year. Symptoms may differ depending on the season SAD occurs:
- Winter-pattern SAD symptoms may include oversleeping, overeating, weight gain, and social withdrawal.
- Summer-pattern SAD symptoms may include insomnia, poor appetite, weight loss, anxiety, restlessness, and episodes of violent behavior.
Atypical Depression
Of the different types of depression, atypical depression is the only one considered a specifier, or subtype, for major depressive disorder or persistent depressive disorder. Atypical depression involves several specific symptoms, including:
- Increased appetite
- Weight gain
- Sleepiness or excessive sleep
- Marked fatigue or weakness
- Moods that are strongly reactive to environmental situations
- Extreme sensitivity to rejection
Psychotic Depression
Psychotic depression is characterized by symptoms of MDD that include episodes of psychosis, such as hallucinations, delusions, or paranoia. Research indicates that MDD with psychotic features affects about four in every one thousand people and is most common between ages fourteen and thirty and in adults over the age of sixty.6
The criteria for diagnosing major depressive disorder with psychotic features involves exhibiting a persistent low mood or lack of interest in everyday life for at least two weeks, four or more other symptoms of depression, and exhibiting symptoms of hallucinations, delusions, paranoia, or psychomotor impairments. Psychomotor impairments involve having slowed thoughts, movements, and lack of feelings.
Causes of Depression
The causes of depression result from a complex interaction between various biological, social, and psychological factors. It is difficult to determine the exact causes of depression, as different depressions have various risk factors. However, research has provided valuable input that may help determine the cause of depression.

Brain Chemistry
One of the most widely accepted explanations for depression is abnormal brain chemistry. In many instances, having too few of certain neurotransmitters in the brain can impact mood and cause symptoms of depression.
Neurotransmitters are chemical messengers in the brain that communicate with each other and are responsible for maintaining brain and body function. Many neurotransmitters produced in the brain play a significant role in mood regulation. Three neurotransmitters are associated with depression:
- Dopamine is responsible for creating positive feelings associated with reward and reinforcement that motivates us. Therefore, reduced levels of dopamine can contribute to depression.
- Serotonin is known as the “feel good” chemical and plays a role in helping regulate mood, as well as contributing to various functions related to the gut, blood clotting, and sexual function.
- Norepinephrine is both a neurotransmitter and a hormone. This chemical is associated with the “fight or flight” response, adrenaline, and helping send messages from one cell to the next. Evidence supports the hypothesis that too little norepinephrine can cause depression, while too much can cause mania.
Hormone Levels
Changes in hormone levels can also affect the development of depression. Hormones are in charge of regulating mood; therefore, changes in hormone levels can greatly impact mental health. Estrogen and progesterone, hormones that are more prevalent in women, have been shown to affect depression and anxiety. This may be a contributing factor to the higher prevalence of depression among women than men.
Family History
Early Childhood Trauma
Those with a history of early childhood trauma or abuse are also more likely to develop depression.
Medical Conditions
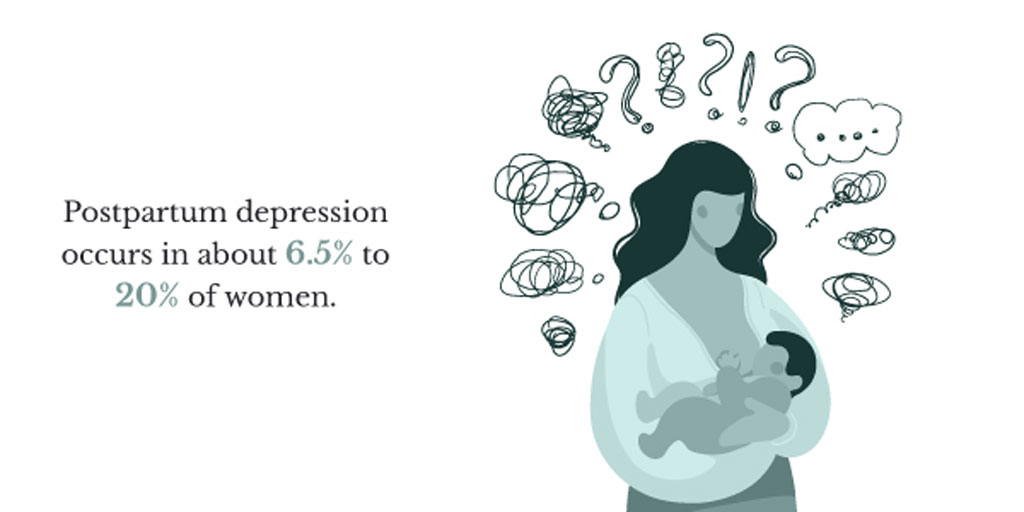
Substance Use
Substance use or misuse can be a contributing factor to experiencing depression. Although drugs and alcohol may temporarily relieve the symptoms of depression, they are ultimately more likely to aggravate or increase depressive symptoms.
Treatment for Depression
There are many different treatment options available to help treat depression. For the best success, many of these treatments are used in combination.
Therapies
Various types of therapy can help treat depression, such as psychotherapy, individual therapy, group therapy, family therapy, and medical therapy.
- Psychotherapy, also known as talk therapy, is an evidence-based therapy that consists of utilizing communication to help various disorders and conditions, including depression.
- Cognitive behavioral therapy (CBT) is a structured therapy that assists individuals in identifying and modifying irrational or maladaptive thoughts contributing to depression. The main premise of CBT is that an individual’s negative beliefs about themselves, the world, and the future contribute to how they think, feel, and act. Therefore, the goal of CBT is to challenge and change these beliefs towards more positive ones.
- Interpersonal therapy (IPT) emphasizes the role of interpersonal relationships and focuses on current interpersonal difficulties.
- Electroconvulsive therapy (ECT) is an effective form of treatment for depression, especially for those with treatment-resistant depression. Trained medical professionals perform ECT in medical settings. Patients usually attend two to three sessions per week for up to twelve sessions in total.
- Light therapy is another form of treatment that is commonly utilized to help treat seasonal affective disorder. Light therapy uses UV light to deliver a therapeutic dose of synthetic sunlight to alleviate depression caused by the seasons. The light given off during light therapy helps to boost melatonin, serotonin, and vitamin D, which may help contribute to better sleep and an increased mood.
What is Psychotherapy?
Medication-Assisted Treatment
Medication-assisted treatment (MAT), such as antidepressants, has proven to be effective in the treatment of depressive disorders. Medical professionals prescribe various medications to patients with depression. Some of these include:
- Selective serotonin reuptake inhibitors (SSRIs) are often the first line of medication used for late-onset depression due to ease of dosing and low toxicity. Some common SSRIs include citalopram, escitalopram, fluoxetine, fluvoxamine, and sertraline.
- Serotonin/norepinephrine reuptake inhibitors (SNRIs) are often used as a second-line medication in individuals who have not responded well to SSRIs. Typical SNRIs include venlafaxine, duloxetine, and levomilnacipran.
- Lithium, anticonvulsants, and antipsychotics are mood-stabilizing medications that effectively treat bipolar disorder and major depressive disorder with psychotic features.
- Atypical antidepressants, tricyclic antidepressants (TCAS), and monoamine oxidase inhibitors (MAOIs) are other types of antidepressant medication used to treat depression.
The type of medication prescribed is determined based on the individual’s side effects, severity of depression, and physical health concerns. Medication should always be discussed with a medical provider.
Support Groups
Many people utilize support groups as a tool to aid in their recovery. There are support groups for a variety of topics, including depression, bipolar disorder, substance use, postpartum depression, trauma, etc. Participating in support groups allows individuals to connect with other people dealing with similar issues, feel acknowledged and supported, and become educated on the disorder.
Support groups can be found online or in person and are available as peer-supported groups or run by a trained professional. There are many support groups available, so it is important for individuals to find a group that supports their needs.
Get Treatment for a Depressive Disorder at Profound Treatment
If you or a loved one has a depressive disorder, Profound Treatment offers a safe, supportive, and inclusive environment. Profound focuses on treating the person, not the disorder. Our trained medical staff utilizes evidence-based treatment approaches to create high-quality and personalized treatment plans to heal the mind, body, and spirit and treat the needs unique to each individual.
For more information about our programs and how we can help you achieve a happy, healthy life, contact us today at 310.929.9546, [email protected], or https://profoundtreatment.com/contact-us/.
Resources
1 https://www.who.int/news-room/fact-sheets/detail/depression
2 https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2011.10091342
3 https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.163.1.109
4 https://www.cdc.gov/nchs/products/databriefs/db379.htm
5 https://www.ncbi.nlm.nih.gov/books/NBK559078/
6 https://www.healthline.com/health/depression/facts-statistics-infographic#prevalence
7 https://med.stanford.edu/depressiongenetics/mddandgenes.html
8 https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-021-03428-3